| المجلد 4 ,
العدد 9
، ربيع الأول 1429 – نيسان (إبريل) 2008 |
| |
| Baseline to be Blastocyst |
| القيمة القاعدية للكيسَةٌ الأُرَيمِيَّة |
| د. زينب إدلبي |
| Edlbi Z. |
| Embryo transfer in human IVF is traditionally performed at the D2- to 4-cells stage, after insemination. When the embryo does not enter the uterus for another 2-3 days, by which time the embryo has develop to blastocyst stage with single blastocele cavity and differentiation into two distinct cell types, (ICM, TE). |
| Main Signs to go blastocyst: |
-Rate of cleavage
-Two cells conceptuses may observed at any time from 20 h post-insemination, usually after 24 h, and may persist until 42 h.
-Viable four-cells pre-embryos are
observed between 39-60 h post-insemination.
-Eight-cells stages are not generally seen until after 54 h but before 72 h.
-In normally fertilization specimens, retard growth (no doubling within 24 h) often indicates reduced viability, so occasionally a pregnancy may be established with a slow-growing pre-embryo, even one found to possess only six to eight blastomeres at 96 h.
-If further cleavage occurs over the next 24h, then the transfer is carried out ,but if no further cleavage occurs, transfer is canceled.
|
| Considerated factors for blastocyst |
1-Environment of lab (Temperature, PH, light);
Fertil Steril, 75(2): 348, 2001,
2-Maternal age;
3-Quality of oocyte;
4-Quality of sperm and source;
Hum Reprod, 11(9): 1963-1965, 1996.
5-Kind of media (Co-Culture, Simple);
6-Concentration of glucose 0.5 mM in media;
Human Reproduction, 14, 3, 774-781, 1999.
Bavister Azuma et la. IVF, ICSI, 1995.
7-Sperm position in oocyte (close to microtubal spindle);
Hum Reprod, 10(3): 484-486, 1995.
8-Position of polar body;
Hum Reprod, 16(2): 306-312, 2001.
9-Safety of pronuclear stage;
10-Early embryo cleavage and compacting;
11-Well responding to gonadotropin;
12-Expand oocyt.
Reproduction, 127, 187-194, 2004.
© 2004 Society for Reproduction and Fertility Fertil Steril, 72(4): 604-609, 1999.
Human Reproduction, 15, 12, 2455-2459, 2000.
|
| Development of Embryo by days |
Day 2: Cleavage stage 2-4 cells;
Day 3: Cleavage stage 6-10 cells;
Day 4: Compacting blastomer.
Early cavitating First sign.
Day 5: Late cavitating Distinct blastocele ICM and TE not laid down
-Early blastocyst Distinct ICM, TE and blastocele Embryo diameter same as day 4 or slightly larger Expanding blastocyst Distinct ICM,
TE, blastocele.
-Expanding blastocyst Distinct ICM-TE, blastocele. Thin zona pellucida Substantial increase in embryo diameter but not fully expanded.
Development embryo to blastocyst from days 2-6.
Day 6: Fully expanded blastocyst Distinct ICM, TE, blastocele. Thin zona pellucida Fully expanded diameter (~215 µm).
-Hatching blastocyst ICM and TE hatching out of zona pellucida -Hatched blastocyst ICM and TE completely hatched out from zona pellucida.
-Empty zona pellucida
ICM = inner cell mass.
TE = Trophectoderm
|
Development embryo to blastocyst from days 2-6.

Compacting Blastomeres Fusing, go to cavitin early
(Compacted to Early blstocyst).
|
|
Early expanding Blastocyst D5 Expanding Blastocyst D5

Blastocyst with very clear Inner Cell Mass

Expanded Blastocyst with clear inner
Completely Hatched Blastocyst D6
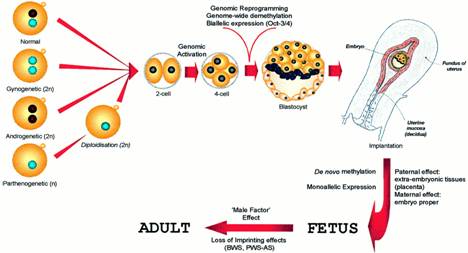
Paternal genomic contributions in blastocyst formation and mammalian development
|
| Conclusion |
-The current recommendations from the American Society for Reproductive Medicine (ASRM) advise that doctors should transfer two or more embryos into women over 35, to enhance the chances of a successful pregnancy. However, transferring more than one embryo can lead to multiple births, which carry a higher risk for both mother and fetus.
-But when the single blastocyst transfer method involves bathing an embryo in a culture of nutrients for five days, until it reaches the blastocyst stage of development the risk will be less. The doctors then determine which embryos are most likely to lead to a successful pregnancy, and transfer them into the woman's uterus.
-Katy Sinclair.
Progress Educational Trust
14 October 2007 Bio News.
|
-blastocysts have proved invaluable for preimplantation genetic diagnosis (Veiga et al., 1997 and to a certain extent in avoiding multiple pregnancies following uterine transfer.
-In order to evaluate the effect of sperm chromosomal abnormalities on pre-implantation development, it is imperative to reconcile what specific contribution the parental genome could possibly have in blastocyst formation
-However, prolonged selection of embryos in vitro (4-5 days), has been proposed to eliminate chromosomal abnormalities, more specifically those inherited by defective spermatozoa. his hypothesis is based upon the assumption that the paternal genetic contribution is indispensable for blastocyst development. This hypothesis and suggest that phenotypic manifestation of paternal genomic abnormalities might not occur prior to implantation.
-In addition to the parent-of-origin effect during embryogenesis, blastocyst transfer may not prevent the inheritance of genetic defects involving 'male factor' loci.
Hum Reprod. 15(12): 2455-2459, 2000.
|
| |
| المجلد 4 ,
العدد 9
، ربيع الأول 1429 – نيسان (إبريل) 2008 |
|
|
|
